Case report - Rare case of Pseudomonas
Koreensis in a Domestic Shorthair cat.
Feline cholangiohepatitis is one of the common causes of feline liver disease; this causes inflammation of the liver and biliary system. The following case report discusses a rare case of Pseudomonas Koreensis causing bacterial cholangiohepatitis in a 3 year old DSH.

Relevant clinical history:
The patient had previously been treated surgically for a hock fracture when he was a kitten. He is an indoor cat in a three cat household with access to outside only when supervised and on a lead and harness. There
is no history of travel outside the UK and he is fed commercially prepared kibble with “Dreamies” as treats. Water is freely available in the house and he is offered nothing other than this to drink.
Presenting signs:
This cat presented out of hours to our first opinion team with clinical signs of anorexia and lethargy which had been non-responsive to meloxicam administration the day before. On clinical examination, he was quiet but responsive, underweight, icteric and mildly dehydrated (estimated 5%). He was pyrexic (temperature 41.1°C), tachycardic (heart rate 192bpm) and showing signs of nausea. Bloods showed an increased total bilirubin (49 ref 0-15mmol/L), mild hypokalaemia (3.1 ref 3.5-5.8mmol/L) and lymphocytosis with a left shift.
Initial treatment:
Intravenous fluid therapy was initiated with added potassium chloride, maropitant was administered for nausea, meloxicam was continued and buprenorphine was started. An ultrasound examination of the abdomen was performed and this showed a small amount of free fluid between liver lobes and a thickened, oedematous gall bladder.
Total bilirubin levels had increased further to 58mmol/L. Co-amoxyclav was started as bacterial cholangitis/cholangiohepatitis was suspected. Abdominal pain was still present despite buprenorphine administration; a fentanyl constant rate infusion was initiated.
Further treatment:
The following day anorexia and pyrexia persisted despite the above treatment and the cat was internally referred. The ultrasound scan was repeated which revealed multiple hypoechoic liver lesions, a hyperechoic gall bladder and similar amounts of free fluid to the previous day. As there had been no improvement with 48 hours of symptomatic treatment, exploratory surgery was planned. Clotting times were checked in-house, these were normal but platelet numbers were slightly low, which was confirmed on a smear. As this was only mild, exploratory surgery was not contraindicated. Gastric and intestinal biopsies were planned as the patient was in poor body condition. As anorexia had persisted, feeding tube placement was indicated.
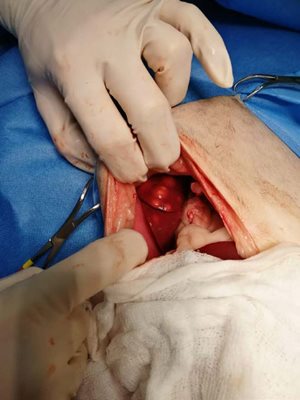
Surgical management:
An exploratory coeliotomy was performed and this revealed multiple liver nodules (up to 1.5cm in size) present on all lobes. The gall bladder was empty and normal in appearance and no gross free fluid was present. The rest of the abdominal organs were examined and no abnormalities were found.
Biopsies and fine needle aspirates were taken from the liver. Liver biopsies were taken using the forceps technique and samples were sent for histopathology and tissue culture. An aspirate of bile was collected and sent for culture and sensitivity.
Following this, gastric, ileal and duodenal biopsies were taken and a gastrotomy feeding tube was placed. The abdomen was flushed, the biopsy sites were examined and no continued bleeding was seen; the abdomen was then closed.

Post-operative treatment:
As co-amoxyclav has been associated with liver damage in humans, a decision was made to switch antibiotic use to ampicillin post-operatively until culture and sensitivity results were available. The cat began eating a few hours after surgery but remained icteric the following morning.
Fine needle aspirate results were consistent with inflammation but a definitive diagnosis could not be reached. Over the following 48 hours jaundice and pyrexia resolved, blood potassium levels normalised without supplementation and the cat could be switched onto sublingual buprenorphine based on pain score. As oral ampicillin was unavailable, amoxicillin was administered.
Results:
- Culture of bile and liver tissue was negative. This could be a false negative result as the patient had been on antibiotics.
Histopathology:
- Incidental helicobacter in gastric mucus.
- Necrotising and pyogranulomatous chronic, multifocal, moderate hepatitis with cholangitis.
- Normal intestinal biopsies.
Further results:
Differential diagnoses at this point included bacterial cholangiohepatitis, TB, FIP and fungal infection.
- ZN staining was negative.
- PAS staining was negative.
- Anti-FIPV antibody was negative.
- Gram staining revealed gram-negative coccobaccilli.
Bacterial cholangiohepatitis was therefore the most likely diagnosis in this patient but culture was negative so we were unable to reach a definitive diagnosis at this point. Yersinia pseudotuberculosis was suspected as this gram-negative coccobaccillus has previously been reported in feline livers causing a nodular, pyogranulomatous hepatitis.
The cat was discharged 4 days after surgery and at regular rechecks he was improving, his liver enzymes and total bilirubin had returned to normal, he was eating well and regaining weight. Therefore, the antibiotics were extended for a total of 6 weeks.
A sample of frozen liver tissue had been stored and this was sent to Great Ormond Street Hospital for 16s rDNA screening PCR. This test revealed that the bacteria was Pseudomonas Koreensis, a rare organism sometimes found in soil.
Discussion:
There is little data available on Pseudomonas Koreensis infection in cats (or other species) so this patient was treated based on clinical improvement. A repeat scan of the liver 6 weeks after the initial scan showed a normal appearance to the liver and antibiotics were stopped at this point.
A follow-up scan 4 weeks later revealed a normal appearance to the liver. It is unknown how this patient was exposed to the organism as outdoor access is closely supervised at all times. To our knowledge, this is the first report of Pseudomonas Koreensis hepatitis in a cat.
Samantha Lane
BVSc BSAVAPGCertSAS MRCVS
If you have a case that you would like to refer to us, please visit the ‘Refer a case’ section of our website.